|
|
||
| Menu | OPAL / AboutOSA | |
|
OPAL Home About People International Collaborators
Opportunities
Events
Related Links
|
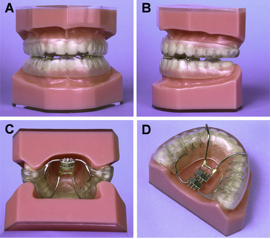
About Obstructive Sleep ApneaObstructive sleep apnea/hypopnea (OSAH) is a common medical condition that causes excessive daytime sleepiness, impaired quality of life and increased cardiovascular morbidity (1). OSAH occurs because of recurrent episodes of partial or complete upper airway obstruction during sleep. Patients are predisposed to develop OSAH because of a narrow upper airway combined with the normal loss of upper airway muscle tone which occurs during sleep. The Role of the Upper airwayThe upper airway is a complex, dynamic, three-dimensional structure and comprises the nasal cavities, pharynx, larynx and trachea. The pharynx forms the crossroads between the respiratory system and the digestive system. It performs diverse functions and participates in swallowing, breathing, speech and defense of the lower airways. At least 24 pairs of muscles act on the pharynx in a complex co-ordinated manner. The pharynx is divided into three segments (nasopharynx, oropharynx, and hypopharynx), according to specific anatomic landmarks. The nasopharynx extends from the rostral limit of the airway to the level of the hard palate, the oropharynx extends from the hard palate to the rostral tip of the epiglottis, and the hypopharynx extends to the level of the laryngeal introitus. The oropharynx can be further divided into two segments: the retropalatal oropharynx, or velopharynx, posterior to the soft palate; and the retroglossal oropharynx, posterior to the base of the tongue. The pharynx is a dynamic collapsible tube whose patency is determined by a balance of pressures (2). The pharyngeal dilator muscles cause a positive pressure (Pmus), which tends to keep the pharynx open. Intraluminal pressure (Plumen), which is negative during inspiration owing to the negative intrathoracic pressure produced by the inspiratory muscles, tends to occlude the pharynx. The pressure at which the passive pharynx closes (Pclose) is determined by the mechanical properties of the airway wall. When the sum of Pmus and Plumen is less than Pclose (Pmus + Plumen < Pclose ) pharyngeal occlusion occurs. Sleep is associated with a reduction in pharyngeal dilator muscle tone (decreased Pmus). Upper airway narrowing increases the inspiratory load and predisposes to upper airway occlusion during sleep (decreased Plumen). In OSAH, the development of areas of segmental narrowing (decreased Plumen) and altered regional mechanics (increased Pclose) appear to be major abnormalities predisposing to upper airway occlusion during sleep. It is well recognised that a minority of patients with OSAH have gross anatomical abnormalities of the upper airway that cause upper airway narrowing. Upper airway imagingUpper airway imaging techniques have been used to assess upper airway size and function in patients with OSAH. These techniques provide important insights into the pathogenesis of OSAH and are also being used increasingly to help individualise therapy for patients with OSAH. These imaging techniques include cephalometry, computed tomography (CT), magnetic resonance imaging (MRI), fluroscopy, nasopharyngoscopy and acoustic reflection. A cephalometric film is a lateral radiographic view of the head and neck in a standard plane with specific emphasis on bony and soft tissue landmarks. Cephalometry has demonstrated a variety of abnormalities of craniofacial and upper airway soft tissue anatomy that may predispose to a narrow upper airway in patients with OSAH and that are related to the severity of the OSAH. Patients with OSAH have been shown to have a small posterior placed mandible, narrow posterior airway space, and enlarged tongue and soft palate and an inferiorly positioned hyoid bone. Posture is an important determinant of both upper airway size and OSAH and many patients report that they sleep better sitting upright than lying in a bed. Several studies have performed cephalometry in both erect and supine positions to examine the effect of posture on the upper airway size and soft tissues. The velopharynx narrows and the tongue and soft palate thickness increases as both normal subjects and patients with OSAH assume a supine position. Early studies with upper airway computed tomography (CT) in awake patients with OSAH confirmed that the airway was narrowing compared with control subjects (5). Fast CT provides the capability of obtaining multiple images during respiration and has demonstrated a significant change in upper size during tidal breathing in awake supine patients with OSAH. Upper airway magnetic resonance imaging is ideally suited to assessing fat distribution or conditions associated with increased tissue water content such as edema (6). Obesity occurs in the majority in the patients with OSAH and is considered to be a major risk factor for its development. Upper airway MRI studies have shown excessive fat deposition in the soft palate, tongue and surrounding collapsible segment of the pharynx in patients with OSA compared with weight matched controls. OSAH treatmentThe treatment of OSAH has to be individualised to each patient and depends on the severity of OSAH and the etiology of the upper airway obstruction. Weight reduction, postural training and relief of nasal obstruction are conservative measures that should be addressed in every patient. Nasal continuous positive airway pressure (CPAP) is the primary treatment for symptomatic patients with OSAH. An example of a CPAP device is shown in figure 1. However, many patients are unable or unwilling to tolerate nasal CPAP therapy on a long-term basis. In these patients, oral appliances (OA) and corrective upper airway surgery including uvulopalato-pharyngoplasty and maxillomandibular surgery have been proposed as alternative therapeutic approaches. Figure 2 shows an example of an OA. OA have been used for many years to correct upper airway obstruction. OA are now widely prescribed for the treatment of mild-moderate OSAH. Mandibular advancement OA are the most widely used type of OA and the degree of mandibular advancement can be specified and subsequently adjusted. Proposed mechanisms of action of OA include increased upper airway size, decreased upper airway collapsibility, activation of upper airway dilator muscles, and stabilisation of mandibular posture. Upper airway imaging has been used to assess changes in upper airway size and function with OA in patients with OSAH. Voluntary mandibular and tongue protrusion has been shown to increase upper airway size and alter upper airway shape. Several studies have demonstrated an increase in the anteroposterior diameter of the upper airway following OA insertion. Kato and associates measured the effect of mandibular advancement on pharyngeal mechanics in paralyzed OSAH patients undergoing general anaesthesia and observed a dose-response effect, indicated by a more negative critical closing pressue (Pcrit) with progressive mandibular advancement. Ng and colleagues studied the effect of mandibular advancement on upper airway Pclose on OSAH patients during sleep and observed a less collapsible airway with mandibular advancement. A variety of predictors of OA treatment success have been proposed. Several upper airway skeletal and soft tissue measurements made from pretreatment lateral cephalometry have been shown to be associated with treatment success. These include a more micrognathic or retrognathic mandible, and a small soft palate and tongue. However, there is considerable overlap between good and poor treatment response with all these variables. Other treatments include pharmaceuticals, neurostimulation, and surgery and have varying levels of efficacy depending upon the patient specifics. Figure 1: Example of a Continuous Positive Airway Pressure (CPAP). Figure used from wikipedia.org. Figure 2: Example of an Oral Appliance. Figure used with permission from Klearway, Inc. References
|
|
| View Edit Attributes History Attach Print Search Page last modified on March 05, 2014, at 03:21 PM | ||